ArrayRx operating principals
ArrayRx’s goal is to provide participating programs with pharmacy solutions that meet their needs.
Backed by strong oversight and governance, public entities have extra confidence in the knowledge that
as a public entity, ArrayRx’s interests are aligned with theirs to ensure program funding is used as
efficiently as possible.
To support its program management goals, ArrayRx has developed fundamental operating principals
that guide the delivery of its services to clients. These principals provide organizations the predictability,
transparency and auditability that are critical to ensuring the wise use of limited taxpayer funds.
Operating principals include:
• Programs designed for public sector and other purchasers
• Fully transparent operations
• Pure pass-through pricing from pharmacies
• 100% pass-through of all manufacturer rebates and fee payments
• Fixed administration fee (per pharmacy paid claim or Per Member per Month)
• Annual market checks performed by an independent third-party consultant
• Comprehensive audit rights
• Ability to customize formularies and clinical services
• Medical and pharmacy alignment and site of care services
Program transparency is validated using detailed performance reports that document the pass-through
nature of its programs, as well as by performing annual market assessments to ensure financial
guarantees are not only being achieved, but that they remain market competitive. In addition, ArrayRx
programs include provisions that support audits of financial terms and performance on contractual
guarantees, claim adjudication, and manufacturer rebates. Independent third-party audits are also
available at reduced rates. These terms ensure that participating programs can be confident that
ArrayRx is working on their behalf
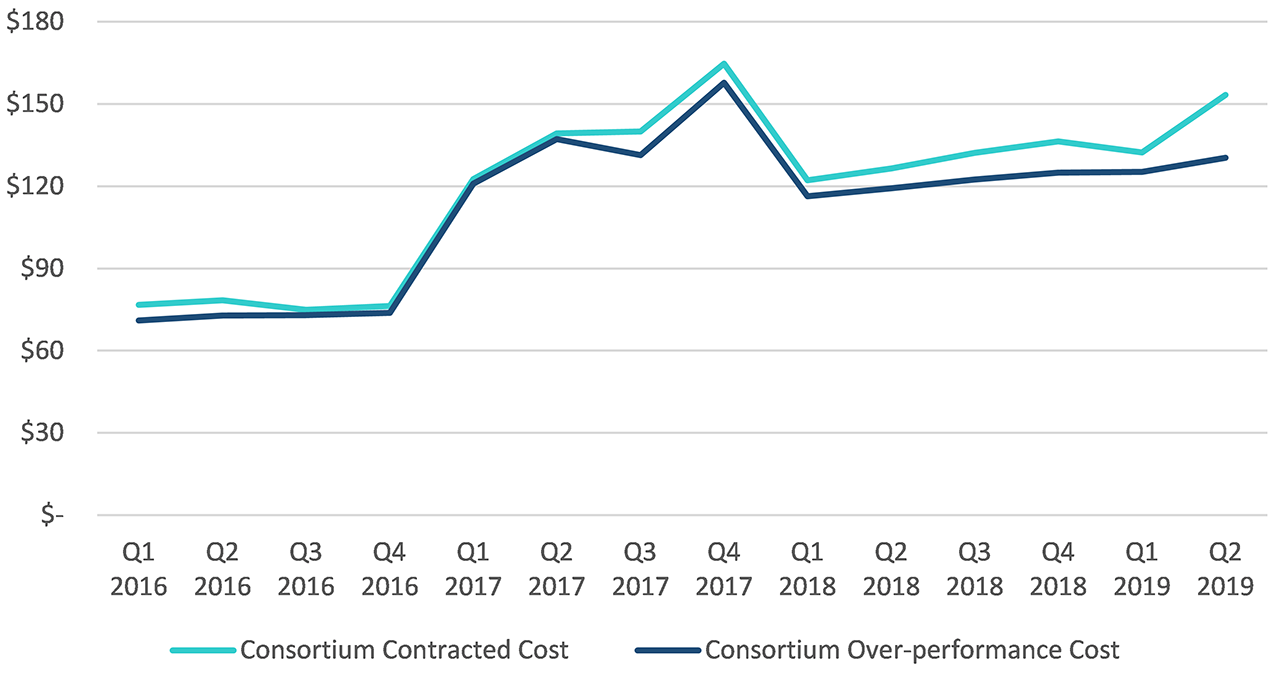
Value of pass-through over-performance
Over $99.4 million in additional savings through network over-performance since 2016
For more information about the Northwest Prescription Drug Consortium, please contact: Pharmacy Program.