Oregon HPV-IMPACT Program through EIP
 On This page:
On This page:
HPV-IMPACT Surveillance Activities
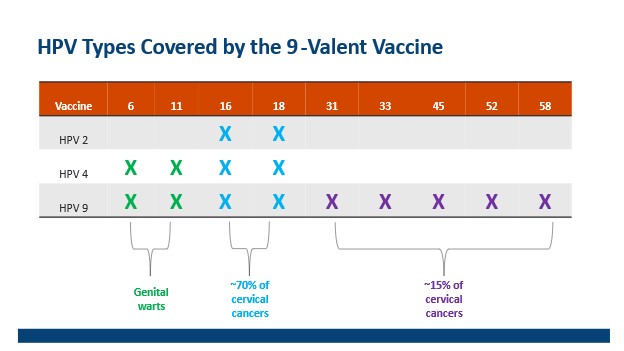
HPV Types Covered by the 9-Valent Vaccine
How Data Is Used
Background
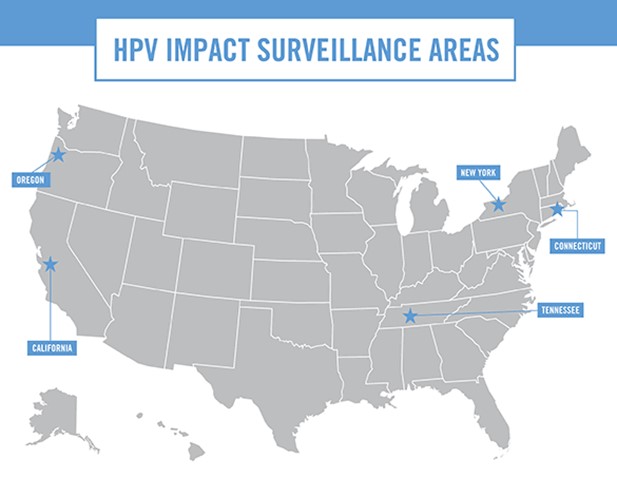
The Human Papillomavirus Impact Monitoring Project (HPV-IMPACT) is a component of the U.S. Centers for Disease Control and Prevention (CDC) Emerging Infections Programs (EIP), a collaboration between CDC, state health departments, and universities.
HPV-IMPACT is a population-based surveillance system that evaluates the impact and effectiveness of the HPV vaccination program by monitoring trends in cervical precancers and cervical cancers.
Why are we concerned about HPV?
- HPV, the human papillomavirus, is the most common sexually transmitted infection
- An estimated 13 million persons are newly infected with a disease-associated type every year in the US
- In the pre-vaccination era, more than 80% of men and women were infected by 45 years old
- HPV causes cancers of the cervix, vagina, vulva, penis, anus, and oropharynx (throat)
- Almost all cervical cancers are due to genital HPV infection, and about 70% are caused by two high risk types, HPV-16 and -18
Number of HPV-Associated and Estimated Number of HPV-Attributable Cancer Cases Per Year in United States
Cancer site
| Gender
| Average number of cancers per year in sites where HPV is often found (HPV-associated cancers) | Percentage probably caused by any HPV typea | Estimated number probably caused by any HPV typea |
|---|
Cervix
| Female
| 11,959
| 91%
| 10,800
|
|---|
Vagina
| Female
| 898
| 75%
| 700
|
|---|
Vulva
| Female
| 4,418
| 69%
| 3,000
|
|---|
Penis
| Male
| 1,381
| 63%
| 900
|
|---|
Anusb
| Total
| 7,854
| 91%
| 7,200
|
|---|
Female
| 5,363
| 93%
| 5,000
|
|---|
Male
| 2,491
| 89%
| 2,200
|
|---|
Oropharynx
| Total
| 21,474
| 70%
| 15,200
|
|---|
Female
| 3,642
| 63%
| 2,300
|
|---|
Male
| 17,832
| 72%
| 12,900
|
|---|
TOTAL
| To
| 47,984
| 79%
| 37,800
|
|---|
Female
| 26,280
| 84%
| 21,800
|
|---|
Male
| 21,704
| 74%
| 16,000
|
|---|
bIncludes anal and rectal squamous cell carcinomas.
Data are from population-based cancer registries participating in CDC's National Program of Cancer Registries (NPCR) and/or the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) Program for 2017 to 2021, covering 98% of the United States population.
For data specific to Oregon, visit the Oregon State Cancer Registry data portal
here.
HPV-IMPACT Surveillance Activities
HPV-IMPACT conducts surveillance for cervical precancers and cancers:
- Cervical intraepithelial neoplasia grade 2 (CIN-2)
- Cervical intraepithelial neoplasia grade 2/3 (CIN-2/3)
- Cervical intraepithelial neoplasia grade 3 (CIN-3)
- Adenocarcinoma in situ (AIS)
- Invasive cervical cancer
We also estimate cervical cancer screening utilization rates and HPV vaccine rates among cases.
![]()
Surveillance Objectives
- Monitor trends in overall incidence of CIN2+ (including precancers and invasive cancer) over time in defined populations
- Monitor prevalence and distribution of HPV genotypes in CIN2+ precancer cases aged 18-39 years and in cancer cases aged≥18 years+
- Estimate and monitor trends in cervical cancer screening utilization among residents of the catchment areas; and
- Estimate the proportion of patients with CIN2+ who received the HPV vaccine and estimate vaccine effectiveness
Surveillance Methods
![]() Figure Represents the Portland Metropolitan 28-zip code Surveillance Area
Figure Represents the Portland Metropolitan 28-zip code Surveillance Area
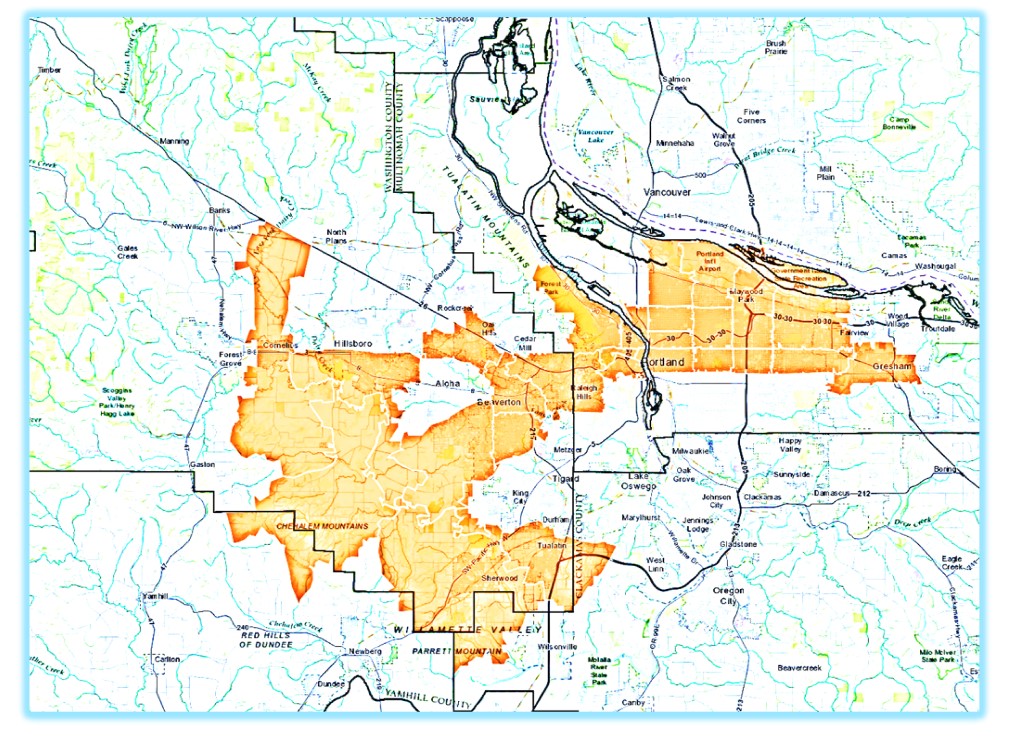
Case Definition: A case is defined as a person at least 18 years of age at the time of diagnosis who is living in a 28 zip code area in the Portland metropolitan area, which spans parts of Multnomah and Washington Counties. Cases must have a histologically confirmed diagnosis of cervical intraepithelial neoplasia (CIN) grades 2 or 3, or adenocarcinoma in situ (collectively referred to as CIN2+) on or after January 1, 2008.
![]() Case Identification: We receive electronic laboratory reports from pathology laboratories. Oregon law,Oregon Administrative Rule 333-010-0032, requires pathology labs to report cervical biopsy reports that show evidence of high-grade dysplasia.
Case Identification: We receive electronic laboratory reports from pathology laboratories. Oregon law,Oregon Administrative Rule 333-010-0032, requires pathology labs to report cervical biopsy reports that show evidence of high-grade dysplasia.
![]()

Data Collection: We conduct-enhanced surveillance for select cases and receive additional information, such as screening history and HPV vaccine history, from provider offices, medical chart review, the Oregon immunization registry (ALERT), the Oregon State Cancer Registry (OSCaR), and
Oregon Vital Statistics data.
Laboratory Methods: To determine the HPV types leading the infection, cervical tissue for CIN cases in women 18-39 years of age and all cervical cancer cases is submitted to CDC for HPV typing. PCR assays is used to detect HPV type-specific DNA. DNA is extracted and tested for 28 HPV types (6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 43, 44, 45, 51, 52, 53, 54, 56, 58, 59, 61, 66, 68, 69, 70, 73, and 82). These types include all types targeted by HPV vaccines and other types that can infect genital tissues. (Note in 2019, manufacture of a 37-type assay was discontinued, and genotyping was switched to the current 28-type assay. The previous assay detected HPV 6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51, 52, 53, 54, 55, 56, 58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73, 81, 82, 83, 84, 89, IS39).
![]()
How Data is Used
We produce estimates of disease burden over time for various population groups, and we measure impact of vaccine on cervical disease. CDC and site partners analyze data and disseminate results in a variety of formats, whether through local, regional, state, national or international conferences, presentations, newsletters, peer-reviewed papers, articles, etc. Our data is used in conjunction with other work to inform policy and evaluate local, state, national, and international goals.
![]()
Department of Health and Human Services (HHS)
National Vaccine Plan Goals:
- Goal 3: Increase knowledge of and confidence in routinely recommended vaccines
- Goal 4: Increase access to and use of all routinely recommended vaccines
CDC Healthy People 2030 Goals:
- Increase the proportion of teens who receive the recommended doses of the HPV vaccine
- Reduce infections of HPV types prevented by the HPV vaccine in young adults
- Increase the proportion of females screened for cervical cancer
- Reduce the overall cancer mortality rates
World Health Organization (WHO) Global Initiative to Eliminate Cervical Cancer – 2030 Targets
- Increase HPV vaccination
- 90% of females receive HPV vaccination by age 15
- Increase screening
- 70% of women screened using a high-performance test by age 35 and again by age 45
- Increase treatment
- 90% of women identified with cervical disease (either precancer or cancer) receive treatment
Select Reports and Publications
- CD Summary
- OSCaR Data Tables:
https://www.oregon.gov/oha/PH/DISEASESCONDITIONS/CHRONICDISEASE/DATAREPORTS/Pages/Cancer-Incidence.aspx
-
HPV type-specific trends in cervical precancers in the United States, 2008 to 2016.
- 1
-
Effectiveness of 1, 2, and 3 Human Papillomavirus Vaccine doses against HPV-16/18 positive High-grade Cervical Lesions. Johnson Jones ML, Gargano JW, Powell M, Park IU, Niccolai LM, Bennett NM, Griffin MR, Querec T, Unger ER, Markowitz LE; HPV-IMPACT Working Group. Am J Epidemiol. 2019 Nov 4. pii: kwz253. doi: 10.1093/aje/kwz253. [Epub ahead of print]
-
Estimated Number of Cases of High-Grade Cervical Lesions Diagnosed Among Women – United States, 2008 and 2016. McClung NM, Gargano JW, Park IU, Whitney E, Abdullah N, Ehlers S, Bennett NM, Scahill M, Niccolai LM, Brackney M, Griffin MR, Pemmaraju M, Querec TD, Cleveland AA, Unger ER, Markowitz LE; HPV-IMPACT Working Group. MMWR.2019 ;68(15):337-3
- 43.
-
Trends in Human Papillomavirus Types 16 and 18 in Cervical Precancers, 2008-2014. McClung NM, Gargano JW, Bennett NM, Niccolai LM, Abdullah N, Griffin MR, Park IU, Cleveland AA, Querec T, Unger ER, Markowitz LE, HPV-IMPACT Working Group. Cancer Epidemiology, Biomarkers, and Prevention, 2019;28(3):602-609.
-
Trends in High-grade Cervical Lesions and Cervical Cancer Screening in Five States, 2008–2015. Gargano J, Park IU, Griffin MR et al. Clin Infect Dis 2019;68(8):1282-91.
-
Increases in Human Papillomavirus Testing Preceding Diagnosis of Cervical Precancer in 5 US States, 2008-2016. Cleveland AA, Gargano JW, Griffin MR, Park IU, Niccolai LM, Bennett NM, Pemmaraju M, Fink D, Brackney M, Scahill M, Ehlers SJ, Unger ER, Markowitz LE; HPV-IMPACT Working Group.J Low Genit Tract Dis. 2021 Jul 1;25(3):192-198. doi: 10.1097/LGT.0000000000000606.PMID: 33797511
-
Cervical adenocarcinoma in situ: Human papillomavirus types and incidence trends in five states, 2008-2015. Cleveland AA, Gargano JW, Park IU, Griffin MR, Niccolai LM, Powell M, Bennett NM, Saadeh K, Pemmaraju M, Higgins K, Ehlers S, Scahill M, Johnson Jones ML, Querec T, Markowitz LE, Unger ER; HPV-IMPACT Working Group. Int J Cancer. 2019 Apr 13. doi: 10.1002/ijc.32340. [Epub ahead of print]
-
Use of claims data to estimate annual cervical cancer screening percentages in Portland metropolitan area, Oregon. Abdullah N, Laing RS, Hariri S, Young CM, Schafer S. Cancer Epidemiol. 2016 Apr;41:106-12. doi: 10.1016/j.canep.2016.01.010. Epub 2016 Feb 18.
-
Monitoring effect of human papillomavirus vaccines in US population, Emerging Infections Program, 2008-2012. Hariri S, Markowitz LE, Bennett NM, Niccolai LM, Schafer S, Bloch K, Park IU, Scahill MW, Julian P, Abdullah N, Levine D, Whitney E, Unger ER, Steinau M, Bauer HM, Meek J, Hadler J, Sosa L, Powell SE, Johnson ML; HPV-IMPACT Working Group. Emerg Infect Dis. 2015 Sep;21(9):1557
- -61.
-
Population-based trends in high-grade cervical lesions in the early human papillomavirus vaccine era in the United States. Hariri S, Johnson ML, Bennett NM, Bauer HM, Park IU, Schafer S, Niccolai LM, Unger ER, Markowitz LE; HPV-IMPACT Working Group. Cancer. 2015 Aug 15;121(16):2775-81.
-
Reduction in HPV 16/18-associated high grade cervical lesions following HPV vaccine introduction in the United States – 2008-2012. Hariri S, Bennett NM, Niccolai LM, Schafer S, Park IU, Bloch KC, Unger ER, Whitney E, Julian P, Scahill MW, Abdullah N, Levine D, Johnson ML, Steinau M, Markowitz LE; HPV-IMPACT Working Group. Vaccine. 2015 Mar 24;33(13):1608-13.
-
HPV type attribution in high-grade cervical lesions: assessing the potential benefits of vaccines in a population-based evaluation in the United States. Hariri S, Unger ER, Schafer S, Niccolai LM, Park IU, Bloch KC, Bennett NM, Steinau M, Johnson ML, Markowitz LE; HPV-IMPACT Working Group. Cancer Epidemiol Biomarkers Prev. 2015 Feb;24(2):393-9.
-
Impact of human papillomavirus (HPV) vaccination on HPV 16/18-related prevalence in precancerous cervical lesions. Powell SE, Hariri S, Steinau M, Bauer HM, Bennett NM, Bloch KC, Niccolai LM, Schafer S, Unger ER, Markowitz LE. Vaccine. 2012 Dec 17;31(1):109-13.
-
Human papillomavirus genotypes in high-grade cervical lesions in the United States. Hariri S, Unger ER, Powell SE, Bauer HM, Bennett NM, Bloch KC, Niccolai LM, Schafer S, Steinau M, Markowitz LE; HPV-IMPACT Working Group. J Infect Dis. 2012 Dec 15;206(12):1878-86.
-
The HPV vaccine impact monitoring project (HPV-IMPACT): assessing early evidence of vaccination impact on HPV-associated cervical cancer precursor lesions. Hariri S, Unger ER, Powell SE, Bauer HM, Bennett NM, Bloch KC, Niccolai LM, Schafer S, Markowitz LE; HPV-IMPACT Working Group. Cancer Causes Control. 2012 Feb;23(2):281-8.
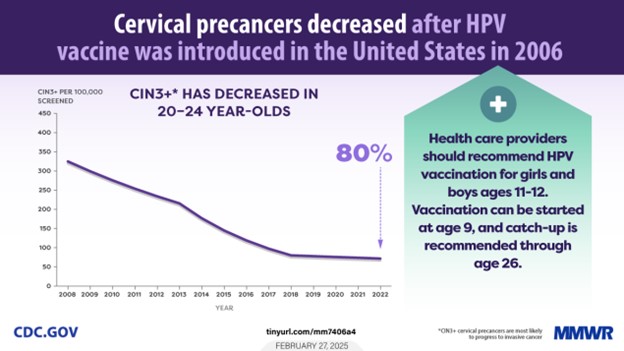
- Trends in Cervical Precancers Identified Through Population-Based Surveillance — Human Papillomavirus Vaccine Impact Monitoring Project, Five Sites, United States, 2008–2022.
Gargano JW, Stefanos R, Dahl RM, Castilho JL, Bostick EA, Niccolai LM, Park IU, Blankenship, S, Brackney M, Chan, K, Delikat EL, Ehlers S, Gonzalez Barrera K, Kurtz R, Meek JI, Whitney E, Vigar M, Unger ER, Markowitz LE; HPV-IMPACT Working Group. MMWR. 2025 Feb 27;74(6):96-101. DOI: http://dx.doi.org/10.15585/mmwr.mm7406a4
- U.S. Women with Invasive Cervical Cancer: Characteristics and Potential Barriers to Prevention. Rosenblum HG, Gargano JW, Cleveland AA, Dahl RM, Park IU, Whitney E, Castilho JL, Sackey E, Niccolai LM, Brackney M, DeBess E, Ehlers S, Bennett NM, Kurts R, Unger ER, Markowitz LE. Journal of Women's Health. 2024 May;33(5):594-603. DOI: 10.1089/jwh.2023.0462. Epub 2024 Apr 12.
Other Important Information
Project Contact
HPV-IMPACT Project Coordinator
Sara Ehlers, MPH
800 NE Oregon St, Suite 772
Portland, Oregon 97232
OHD.ACDP@oha.oregon.gov
HPV-IMPACT Staff
Dr. Emilio DeBess – HPV-IMPACT Principal Investigator
Kameny Chan, MPH – Epidemiologist
Sara Ehlers, MPH – HPV-IMPACT Project Coordinator
Bradley Beauchamp – Electronic Publishing Design Specialist