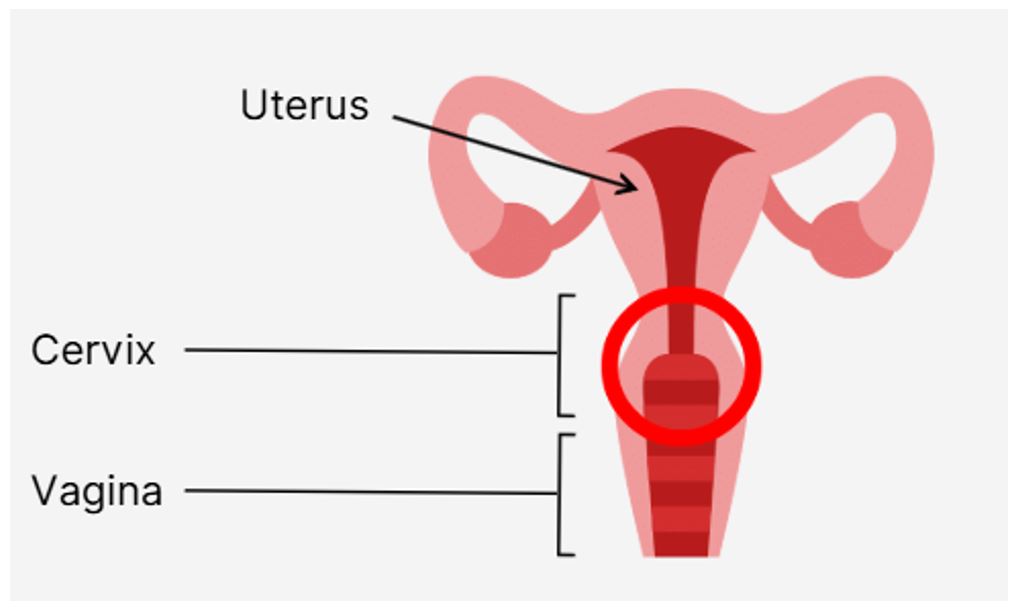
What is the cervix? The cervix is the lower part of the uterus that connects to the vagina. You can think of it like a doorway between the uterus and the vagina.
|
Figure 1: HPV and the Cervix: Know the Connection
|
What are cervical precancers?
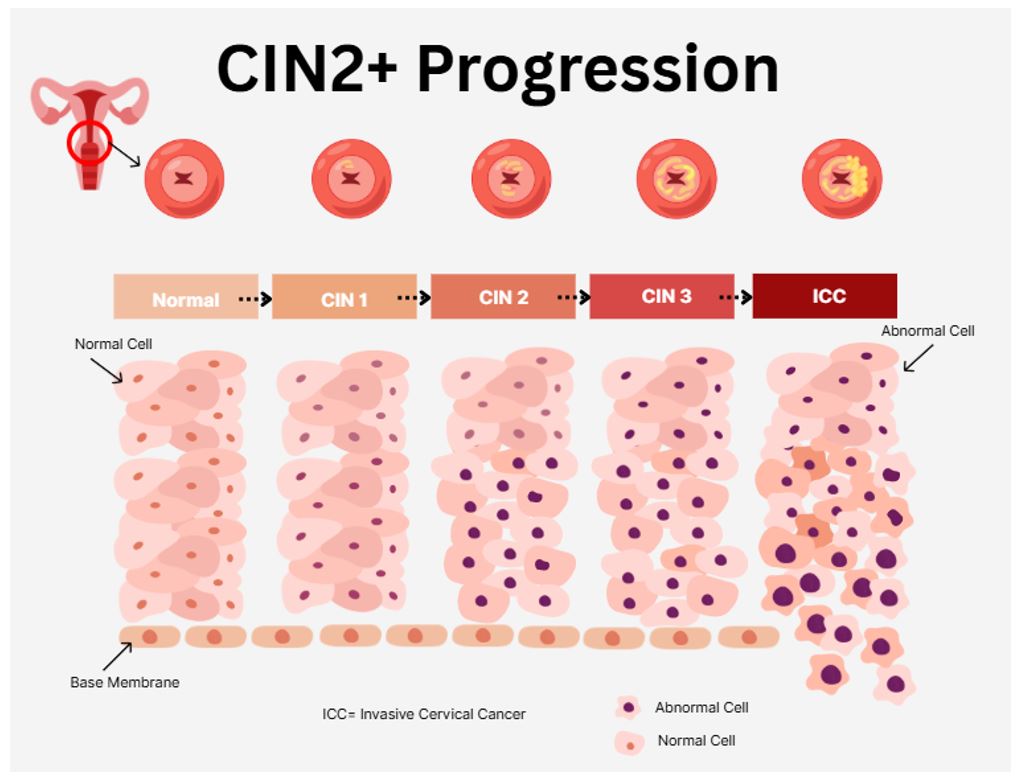
Cervical precancer, also known as cervical intraepithelial neoplasia (CIN), is when abnormal cells grow on the surface of your cervix, especially when it is infected with Human Papillomavirus (HPV). If these abnormal cells are not treated, they could turn into cervical cancers.
Figure 2: This figure shows how abnormal cell changes in the cervix,
known as CIN2+, can progress to cervical cancer if not treated
|
1. How is it linked to HPV? 91% of cervical cancer is linked to Human papillomavirus (HPV) (ADD CITATION CDC). In additional to cervical cancer, HPV can cause other type of cancers such as vulvar, vaginal, penile, anal and oropharyngeal (throat) cancers.
HPV is a very common virus; it is the most commonly sexually transmitted infection in the United States (CDC).
Most HPV infections go away on their own. However, some infections can persist and lead to cervical cancer. HPV is a recognized cause of cancer. Although most HPV infections are asymptomatic and clear spontaneously, persistent infections can progress to precancer or cancer.
|
2. HPV types
There are over 200 types of HPV, and over 40 types of those infect the genital tract. CDC has identified 14 types as high risk for causing cancers. HPV types 16 and 18 are the most common high risk types and are responsible for causing about 70% of cervical cancers.
3. Symptoms of cervical precancer
Most people with pre-cervical cancer have no symptoms. That’s why regular cervical cancer screening is important. Pap Smears and HPV Testing should be done regularly.
4. Can cervical precancer and cervical cancer be prevented?
Yes. It can be prevented by regular cancer screening and HPV vaccines.
5. Cancer Screening Guidelines
Age 21-29
-Pap test every 3 years
-HPV testing is not recommended alone
Age 30-65
HPV test alone every 5 years or
PAP smear alone every 3 years or
HPV and PAP smear (Co-testing) every 5 years
Screening may stop after age 65 if there is no abnormal test result in history and no history of cervical cancer
6. HPV vaccines
HPV vaccine protects against the most common high-risk HPV types, including those that cause cervical cancer. It is recommended to get vaccinated at ages 11 or 12 years (can be given as early as 9) until the age of 26 years. For people ages 27-45 years, the vaccines can be given based on discussion with healthcare providers.
Key takeaways
Pre-cervical cancer isn't cancer, but it is a warning sign (and a requisite step to cancer). Early detection through HPV testing and Pap smears, along with vaccination, saves lives.