Congenital syphilis is a crisis in Oregon.
10/8/2025
Syphilis is a sexually transmitted infection (STI) that can cause
serious health problems without treatment. Rates of syphilis in Oregon have decreased in the last two years. But, the rates of syphilis diagnosed during pregnancy have increased during that time. Congenital syphilis occurs when syphilis passes from a pregnant person to their fetus. An increase in these rates means more infants are born sick.
In 2014, Oregon recorded two cases of congenital syphilis.
In 2024, that number rose to 44.
How is syphilis spread and treated?
Syphilis spreads through sexual contact or from a pregnant person to their fetus during pregnancy or childbirth.
Historically, syphilis has mostly been found in men, but rates of cases in women have risen in recent years.
Syphilis affects some communities more than others due to systems that do not work for everyone .
In February 2025, Dr. Pete Singson, Medical Director for Oregon Health Authority (OHA)'s HIV, STD and TB Section, wrote a
letter to Oregon healthcare providers. He emphasized that the burden of congenital syphilis disproportionately impacts pregnant people of color and those who experience housing instability, have criminal justice involvement, and/or use drugs. Importantly , Dr. Singson attributes these differences in the burden of congenital syphilis to systems that do not work for everyone.
“It is critical to understand that these disparities are not due to race or ethnicity, but rather by the compounded effects of systemic racism, poverty, houselessness, incarceration, substance use, and stigma," wrote Dr. Singson.
Congenital syphilis is preventable and curable.
Syphilis during pregnancy can cause miscarriage, stillbirth, and prematurity. Babies born with congenital syphilis can be born with physical defects and long-term neurological problems.
This is why it is so important to prevent congenital syphilis by screening and treating syphilis in pregnant people.
Oregon's public health system is working to prevent congenital syphilis and protect future generations.
OHA monitors trends related to syphilis, congenital syphilis and other STIs. OHA's HIV, STD and TB section supports prevention, testing and treatment efforts. It also supports partnerships between community-based organizations (CBOs) and local public health authorities (LPHAs).
OHA, LPHAs and community partners around the state are working together to help achieve statewide goals to reduce syphilis and congenital syphilis. Here is a snapshot of some of this ongoing work.
Expanded screening
Screening means checking for syphilis even when a person is not showing symptoms. OHA guidelines advise healthcare providers to screen patients for syphilis at least three times during pregnancy:
- At the first prenatal visit or presentation to care in pregnancy
- At 28 weeks
- At delivery
OHA also recommends screening all patients with no or limited prenatal care for syphilis at any opportunity. Screening ensures the highest likelihood of detecting and treating syphilis before the pregnant person delivers.
OHA encourages emergency departments, urgent care centers, and other sites that see people who don't receive regular medical care to implement “opt-out" screening for syphilis. This means checking for syphilis unless a person declines.
Public health partnerships help address congenital syphilis.
Partnerships between OHA, LPHAs, CBOs and healthcare providers are essential to reach all communities around Oregon with information and resources to prevent syphilis. Below are two examples of how county health departments are partnering with community partners and healthcare providers to screen for and treat STIs, including syphilis.
Lincoln County Public Health Department partners with Lincoln County Jail to provide STI testing, education, referrals and information (in English and Spanish) to people in custody.
“Adults who are in custody are at higher risk of getting sexually transmitted infections and would not have access to testing if it wasn’t for our public health nurse who comes in to provide testing and information.” - Lincoln County disease prevention and harm reduction program manager

A Lincoln County Public Health staff member administers a syphilis test.
Read more about how Lincoln County is working to reduce the spread of syphilis here.
In Clackamas County, the public health department created a communications toolkit with information and resources to help clinical and non-clinical partners prevent congenital syphilis. The toolkit includes social media posts, digital resources, and print materials to help partners spread the word about screening and treatment resources across the Portland metro region.
"Community voice was central to developing these materials. We built this campaign around feedback from community members with relevant lived experience, ensuring the message truly reflected and resonated with the people of Clackamas County." - Malley Nason, sr. program planner, Clackamas County Public Health
You can find the toolkit as well as request free, professionally printed materials for your organization here:
www.clackamas.us/publichealth/syphilis-toolkit
To ensure state and local efforts to prevent congenital syphilis continue, investment both federally and locally is necessary.
Learn more about how Oregon public health is working to address syphilis.
As rates of preventable diseases increase, improving vaccination rates is more important than ever. Oregon’s public health system is working on it.
5/14/2025
Rates of vaccine-preventable disease have risen in recent years.
Oregon saw 1,175 cases of pertussis (also known as whooping cough) reported in 2024. This was the highest number of cases reported in a single year since 1950, when 1,420 cases were reported.
Pertussis can make people very sick, and in some cases, lead to hospitalization or death. Children and infants are most at risk of serious illness or death.
Pertussis is a vaccine-preventable disease – meaning just that: it can be prevented. Getting vaccinated is the best way to avoid contracting the disease. Although it is possible for vaccinated people to get pertussis, the vaccine’s protection goes far beyond the first line of defense.
Research has shown that being vaccinated against pertussis can reduce the risk of severe disease by as much as 60%.
Vaccination against pertussis is included in the
4:3:1:3:3:1:4 series. Also called the two-year-old vaccination series, these vaccines are recommended for all children by the time they turn two.
Two-year-old vaccination rates were rising in Oregon for nearly a decade before COVID-19 hit and rates began to fall. The reasons for this decline are not entirely clear, but contributing factors may include COVID-19’s strain on the health care system, vaccine hesitancy and misinformation. Increased social distancing and masking during this time also lowered the risk of exposure to pertussis and other communicable diseases, leading people to view the vaccine as less important.
Systemic barriers to access contribute to lower immunization rates among Oregon’s communities of color.
Even before vaccination rates began falling in recent years, Oregon has experienced significant immunization rate disparities. Communities of color are less likely to be vaccinated and more likely to get sick with vaccine-preventable diseases compared to white communities. White residents are vaccinated at a higher rate than the state’s average, and residents who are Black or African American, American Indian or Alaska Native, and Hawaiian or Pacific Islander are vaccinated at lower rates than the state’s average. OHA strives to close these gaps as part of its goal to eliminate health inequities in Oregon by 2030.
Collaborative efforts to prevent and respond to outbreaks occur locally and statewide.
OHA, local public health authorities (LPHAs), community partners and health providers are working together to make higher vaccination rates a reality by providing culturally relevant outreach and education and making vaccines easier to access.
Easier access can happen through things like:
- Using mobile vaccine clinics to bring vaccines to people who are homebound, residents of long-term care facilities and people who live in rural areas
- Setting up mobile vaccine clinics where people need to go anyway – like grocery stores, schools, places of worship, parks, community centers and office buildings
- Offering vaccines at community events like festivals, music performances and street fairs
- Offering translated materials and interpretation services at vaccine events
- Partnering with community organizations to share culturally and linguistically relevant information with the communities they serve
- Partnering with faith-based organizations and faith leaders to share vaccination information and host vaccine events
These are some examples of this work around Oregon:
- In Crook County, the LPHA partners with schools and HeadStart programs to reach students and parents by offering immunizations at school parent nights.
- In Clackamas County, the LPHA partners with culturally specific organizations to get the word out about immunizations. Recently, the Ukrainian Foundation created a video featuring Clackamas County Public Health’s Eastern European Liaison speaking in Ukrainian about childhood immunizations.
- The Multnomah County Immunization Team partners with the Community for Positive Aging to host vaccine clinics and share information. In October, the Immunization Team presented and answered community members’ questions about the new COVID-19 vaccine formulation.
Programs like Vaccines for Children promote health equity by removing cost as a barrier to vaccination.
The
Vaccines for Children (VFC) program provides free vaccines to kids whose parents may not be able to pay for them. It operates all around the country and provides vaccines to over 50% of Oregon’s children. VFC was created in response to the
1989-1993 measles epidemic in the United States, in which over half of the children infected were found not to have been vaccinated against measles.
Congress passed the
Omnibus Budget Reconciliation Act of 1993, and the VFC program was born. The VFC program provides the vaccines to a nationwide network of public and private providers who administer the program locally. In Oregon, the CDC-sponsored Immunization Quality Improvement for Providers (IQIP) program supports VFC-enrolled partners by helping providers assess current practices, review immunization rates and set evidence-based, achievable goals for improvement.
The success of the IQIP program – which includes federal, state, county, provider and community partners – highlights the power of collaboration across the public health system.
In Deschutes County, Deschutes County Public Health (DCPH) staff used the IQIP program in gathering local clinics to form a community of practice. The group met quarterly, with each clinic developing immunization rate goals and implementing diverse interventions focused on using clinical data to reduce missed opportunities to vaccinate, catching up children who were behind on vaccinations, and streamlining processes to improve rates. From 2016 to 2020, participating practices raised immunization rates by more than 8 percentage points. Although most IQIP programs – including in Deschutes County – were paused when COVID-19 started, the program is regaining momentum and efforts are resuming around the state.
Learn more about how Oregon tracks immunization rates:
- The Oregon Immunization Program keeps
this dashboard up-to-date with immunization data.
- Check out the
2024 Oregon Public Health Accountability Metrics report to learn more about how immunizations fit into the public health system’s work to ensure that it is improving health, eliminating health inequities and effectively using public dollars through a modernized health system.
Building resilience: How Oregon tackles extreme weather's health risks
10/18/2024
Extreme weather in Oregon: A call for climate resilience
Oregon's climate isn't what it used to be. Summers are hotter, wildfires are more intense, and droughts seem to stretch on forever. These extreme weather events are our new normal, and for most of us the most striking impacts of climate change. They bring a wave of challenges that affect the health of our families and communities and deepen existing health inequities. This means the people most impacted by racism, poverty, and prejudice are also hit the hardest by extreme weather.
Our 2023 annual
Climate and Health in Oregon Report shows how these climate threats facing our state affect the health of people who live here.
Read the full report:
2023 Climate and Health in Oregon Report.
Human impacts and human-centered solutions
These climate threats aren't just about rising temperatures—they're about real people facing real health risks:
- Heatwaves endangering the lives of community members, especially older adults living alone and with low incomes.
- Wildfire smoke polluting our air, leading to a spike in asthma and heart problems.
- Droughts threatening our water supply, making clean drinking water harder to come by.
If you've been through a wildfire or had another extreme weather event hit close to home, this can be hard to read. It's personal. Sometimes, knowing what's coming helps, as well as having a role in the solution. This blog will both describe the health harms of extreme weather in Oregon and talk about what we can do to support a healthy future.
The good news is that we can work together to support community health in the face of these challenges.
Coming together to build resilience to extreme weather events
To tackle these challenges, we've teamed up with partners across the state—from community-based organizations to local health authorities. Together, we're building a resilient public health system that's ready for whatever mother nature throws our way.
Our long list of partners includes:
- Local public health authorities (LPHAs)
- Community based organizations (CBOs)
- Regional coalitions
- Health care and behavioral health providers
- Public safety agencies
- Faith-based institutions
- Schools
- Environmental agencies
- The business sector
Together, we're building climate resilience by:
-
Responding to and preparing for health impacts: More frequent wildfires, heat waves and other extreme weather events are challenging our health systems like never before.
-
Planning for chronic health stressors: Poorer air or water quality have cascading impacts on mental health, food, access to healthcare, housing, income, transportation and other aspects of well-being.
-
Leading with equity: We are working to address the health, social and economic systems that contribute to making certain communities more vulnerable to climate-associated health risks.
Read on to learn how climate is challenging our communities, and what we can do about it.
Extreme heat: The health impacts of rising temperatures
If you've noticed that summers feel hotter than they used to, you're not alone. The year 2023 was the hottest on record globally. In Oregon, extreme heat events—those days when temperatures soar above normal—are happening more often and with greater intensity.
Here's the reality:
-
June 2021: An extreme heat event hit the Pacific Northwest, leading to 102 deaths, mostly among isolated, low-income older adults.
-
Rising temperatures: This trend isn't going away. As temperatures rise, so does the risk of heat-related illnesses and deaths.
Daily heat-related illness emergency department and urgent care visits and maximum daily heat index in Oregon, May-September, 2023.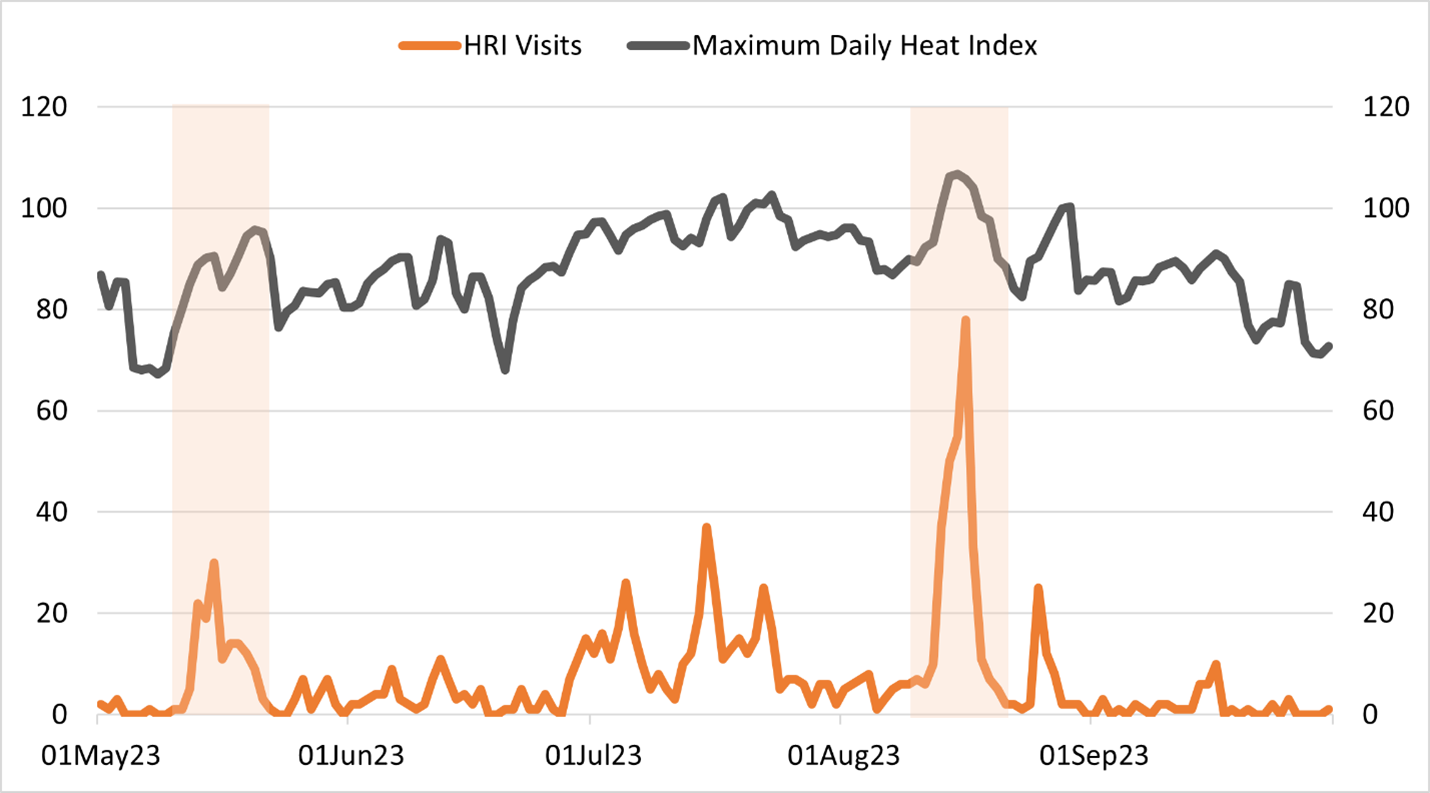
Air quality: The health impacts of wildfire smoke
Wildfires are becoming larger and more severe, creating smokier air that can impact Oregonians' lung health and heart health.
The facts:
-
Respiratory health: In 2023, respiratory illness rates in some Oregon communities were nearly double the state average due to poor air quality. The following communities faced the most extreme impacts:
- American Indian/Alaska Native
- Black/African American
- Native Hawaiian/other Pacific Islander
-
Long-term impact: The particles in wildfire smoke can cause both immediate and long-term health issues, including asthma and heart attacks.
These numbers aren't just statistics – they represent real people struggling to breathe.
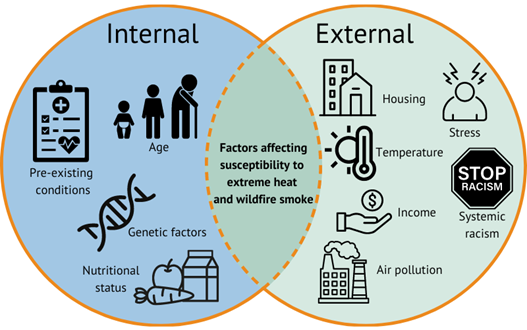
Factors affecting susceptibility to extreme heat and wildfire smoke.
Water security: When the wells run dry
Across Oregon, more frequent and severe droughts, floods and growth of toxin-producing algae in water are threatening our water security—the ability to access clean, safe and affordable water.
Key concerns:
-
Drought: In 2023, 52 percent of Oregon experienced severe drought, with 30 percent facing extreme conditions.
-
Waterborne diseases: Rising temperatures and water scarcity are creating perfect conditions for diseases like Lyme Disease and West Nile Virus to spread.
Mental health: The hidden toll
While physical health impacts are more visible, the mental health toll of climate change is just as real. This can look like anxiety about the future or the trauma of losing homes and livelihoods to wildfires.
What we're seeing:
-
Youth anxiety: The
2022 Climate Change and Youth Mental Health Report revealed that many young people in Oregon are struggling with feelings of hopelessness and despair about the future.
-
Community impact: Extreme weather events are leading to increased rates of anxiety, depression and post-traumatic stress disorder (PTSD).
Oregon youth reporting feelings of anxiety, frustration and hopelessness about the future is a sobering reminder that extreme weather affects us all, in ways both seen and unseen.
Building resilience: Our path forward
Over the past several years, we've developed a resilience framework that's all about relationships—between public health, housing, healthcare, forestry, land use and community partners. This isn't just about physical infrastructure; it's about people and the connections that make our communities stronger.
Oregon Public Health Modernization funding is the backbone of this effort, providing resources that organizations need to build these vital relationships, innovate and work together toward a common goal of climate resilience.
Here is how the work is playing out across our state.
Community-based organizations: The heart of resilience
Supported by health modernization funding, community-based organizations (CBOs) across Oregon are stepping up to meet climate challenges head-on.
Spotlight:
Many CBOs have also partnered with LPHAs to respond to extreme weather events. In 2020 and 2021, Northwest Family Services and Clackamas County Public Health Division helped residents evacuate from wildfires. In 2022 and 2023, they expanded their efforts to distribute air-conditioning (AC) units to those in need—providing not just relief from the heat, but a lifeline. Learn more about the partnership in this video:
Northwest Family Services and Clackamas County Public Health Division partnership video
Local public health authorities: On the front lines
Local public health authorities (LPHAs) are crucial in this fight, working with partners to create action plans tailored to their communities.
Spotlights:
Tribal communities: Protecting heritage and health
For Oregon's nine federally recognized tribes, modernization funding is helping to preserve both health and cultural heritage.
Initiatives:
Oregon Health Authority: Supporting resilient communities
At OHA, we are centering equity in our efforts to modernize statewide public health infrastructure. This includes investments in climate equity, healthy homes and schools, land use and health, healthy waters, and epidemiology (the study of how health outcomes affect populations and why).
A few of our initiatives:
-
Grant funding: Programs like
the Healthy Homes Grant Program help low-income households and those impacted by environmental justice factors equip their homes to withstand environmental hazards like harmful air quality and extreme heat.
-
Air conditioner and air filter distribution: We also administer a program to distribute
air conditioners and air filters to Oregonians in need, helping them protect themselves from extreme heat and wildfire smoke.
OHA leads the state with investments in climate resilience, funding and technical support to our public health partners, and data tracking systems related to climate and health. These supports are not always the most visible, but we believe they are vital. They lay the foundation for our partner organizations as they innovate and work together toward a common goal of climate resilience.
Partnering for a healthier future
Addressing the impacts of extreme weather on public health is a critical priority for Oregon's public health system. By working together—through proactive measures and strong community partnerships—we can protect the health and well-being of all Oregonians. Continued investment in public health modernization is essential to meet these challenges head-on and ensure a healthier future for our state.
Make a difference in Oregon
You can be part of this journey. Here's how:
- Subscribe to our e-newsletters for updates on public health initiatives.
- Share this information on social media to spread awareness.
- Get involved: Support local public health initiatives and policies.
Through resilience and collaboration, we can face Oregon's climate challenges together - ensuring a safe, healthy and equitable future for all.